Marathon Runner
Robert Fletcher, 48
Husband/ Father/ Police Officer
Hello everybody! My name is Robert, I am 48 years old and originally from Yorkshire, but have lived in Leicestershire since 1998 due to work and family commitments. Currently, I work as a Police officer for Leicestershire Police.
I have been married for just over 6 years to my wonderful wife, Maria Fletcher nee Gavriel. Some of you may already know her from when she undertook the role of committee secretary for the UKTS. During her two years working for the society, she organised many successful and profitable charity events.
I am a father to my fifteen year old teenage daughter and owner of three dogs and a cat, so you can only imagine what our home is like sometimes!
Since leaving the Army way back in 1997, I have been invested in my fitness. Prior to lockdown, I had been undertaking training at Leicester Kickboxing Club. Martial Arts is one of those exclusive sports that has changed my life and helped me to continuously learn about myself and other people. For the last four years I have been a member, training in K1 Dutch kickboxing style. Running and cycling are also a favourite pastime of mine. Recently, I have proudly completed a charity event raising money for the Motor Neurone Disease Association. Partaking in the ‘7in7’ challenge, which consists of running seven miles everyday for seven consecutive days, I ran a total of 49 miles.
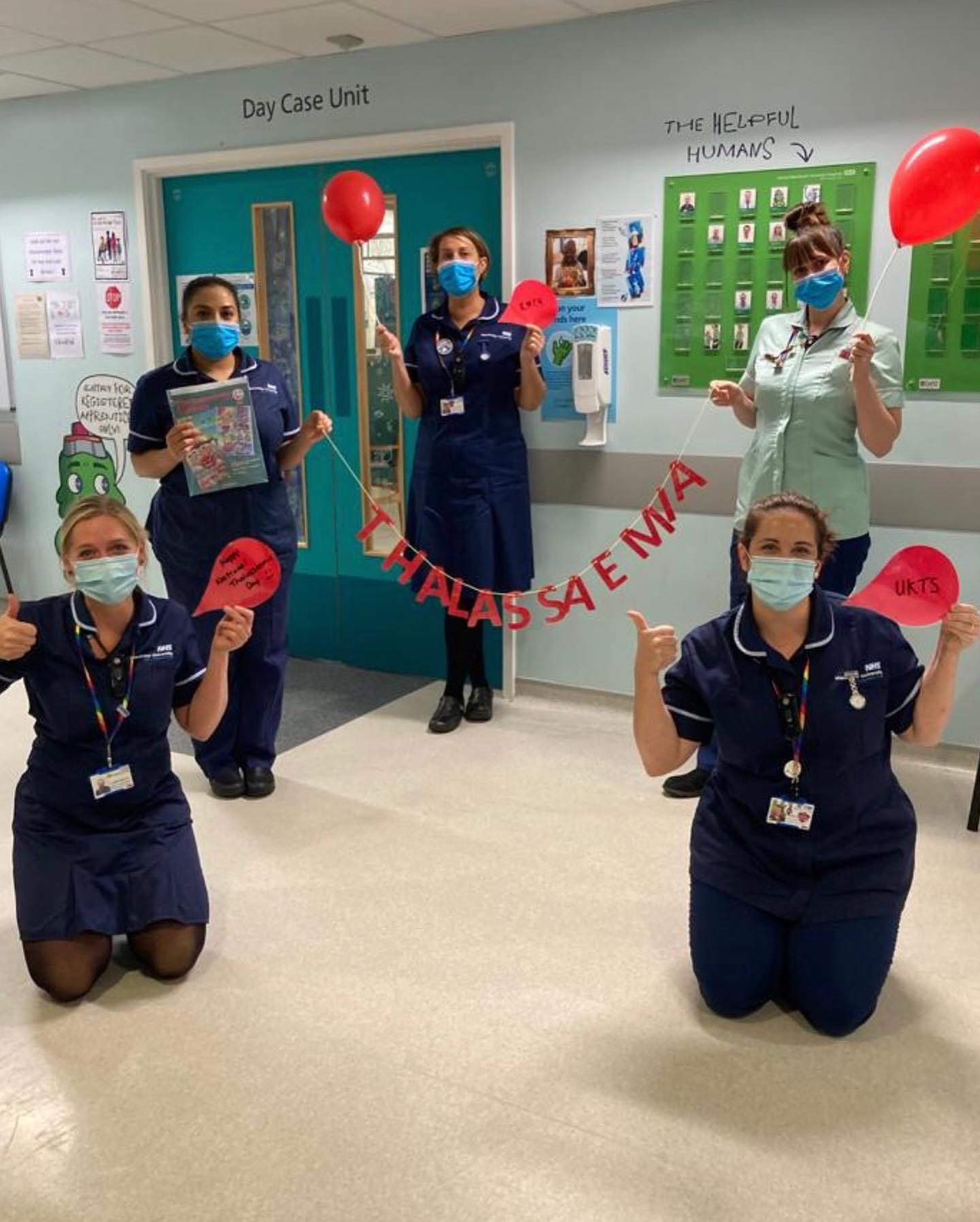
One of the main reasons why I have decided to run the London Marathon for the UKTS is because of my wife Maria, who lives with thalassaemia major. Prior to meeting her, I had never heard of thalassaemia as well as being unaware of its further complications and how it impacts the day to day lives of sufferers. I have been truly inspired and privileged to see how Maria goes about maintaining some normality within her daily life. She attends many medical appointments and maintains and runs a busy home life; all with a smile and a positive can do attitude. Through Maria, I have become friends with some of the Greek Cypriot thalassaemic community. They have been my inspiration to get myself off the sofa, put my best running shoes on and get out there to raise as much money as possible because they all deserve the best quality of life. I have been truly humbled by their positivity and great sense of humour that derives through personal battles and ongoing adversity.
The only marathon I have ever ran was a half marathon back in 1991, in West Berlin. Aged 17 and a soldier. I remember my Platoon Sergeant the day before saying to me ‘Fletcher, make sure you are dressed in civilian kit and parade outside the guardroom prompt and sharp Sunday Morning! Someone’s dropped out through injury’. Back then, my training consisted of consuming less quantities of German beer than normal for a Saturday night.
Now it is not that easy. Simply looking at my trainers for too long will cause me to end up with blisters and break into a sweat. Anyway, it’s all in the planning, so I will be starting a structured training plan in June to get marathon fit for October 3rd and do the UKTS proud.
At the moment, I run about twice a week with the distance varying from 4 to 8 miles. I also mix some kickboxing training sessions into my routine that consist of skipping, shadow boxing and finishing off with punching and kick combinations on the punch bags.
I feel very honoured and privileged to represent and raise money for the UKTS during the London Marathon. Hopefully, you are there on the day to cheer me on, it would be great to meet you all after to celebrate!
I encourage you all to donate what you can, a little really goes a long way and I will be so grateful to every one of you.